- HOME
- Market Insights
- Is Your Gut Your Second Brain? How It Affects Your Whole Body
Is Your Gut Your Second Brain? How It Affects Your Whole Body

Here's something you might relate to: stress hits, and suddenly your stomach's in knots. Or you're constipated for a few days, and boom—your skin breaks out and your mood crashes. These symptoms seem random, right? Actually, they all connect back to one organ: your gut.
The Netflix documentary "Hack Your Health: The Secrets of Your Gut" got people worldwide talking. It reveals something fascinating—your gut does way more than digest food. It affects your immunity, mood, and even your weight. Scientists now know the links between your gut, brain, and immune system run deeper than anyone imagined. That's why it's called your "second brain."
Research shows that healthy habits (including caring for your gut) can significantly lower your risk of chronic diseases. This often-overlooked organ deserves more attention.
References: PMC5808284, MDPI-IJMS 26188905, PMC: 28523941, PMC10699709, Frontiersin: The gut microbiota, UCLA Health: Serotonin
Quick Navigation
Why Is Your Gut Called the "Second Brain"?
Your Gut Has Its Own Nervous System
Get this—your gut contains hundreds of millions of nerve cells. That's more than your spinal cord! This network, called the "enteric nervous system," works independently. It controls digestion and gut movement without needing orders from your brain.
Here's the really interesting part: the majority (often described as approximately 90%) of your body's serotonin is linked to your gut. Serotonin is that feel-good chemical that keeps you happy and calm. When your gut isn't happy, your mood takes a hit—and this isn't just in your head. It's actual physiology at work.
Certain probiotics (like Lactobacillus and Bifidobacterium) can boost neurotransmitter production, helping stabilize your mood and sleep patterns.
How Do Your Gut and Brain Talk to Each Other?
Your gut and brain share a two-way highway called the "gut-brain axis"—think of it as a constant conversation happening through nerves, hormones, immune signals, and metabolic products. This affects your mood, thinking, sleep, and overall health. A 2025 Nature Communications study shows this pathway works through four main routes:
1. The Vagus Nerve Highway
Here's something surprising: 80% of signals flow from your gut to your brain. Chemical signals from your gut microbes travel up the vagus nerve, affecting how your brain handles emotions and stress.
2. Hormones and Neurotransmitters
Your gut bacteria prompt intestinal cells to make substances like GABA. These travel through your bloodstream or nerves to your central nervous system, regulating your mood, sleep, and appetite.
3. Metabolic Byproducts
When gut bacteria ferment dietary fiber, they create short-chain fatty acids (like acetate, propionate, and butyrate). These compounds fuel your intestinal cells, strengthen your gut barrier, regulate inflammation, and improve brain function.
4. Immune Response
Your gut houses about 70% of your immune cells. When your gut microbiota diversity drops or balance shifts, things go wrong—dysfunction kicks in and inflammation risk climbs. A weakened gut barrier lets toxins leak into your bloodstream, triggering chronic inflammation that can affect brain health and contribute to conditions like depression and Parkinson's disease.
Real-World Examples
A 2019 study found something eye-opening: Parkinson's patients showed gut microbiota abnormalities years before developing tremors or slow movement. Recent research suggests that gut bacteria imbalances might send harmful proteins to the brain via the vagus nerve. This explains why many Parkinson's patients face constipation early on.
A 2025 study also found that kids with more diverse early-life gut bacteria show more stable emotional and cognitive development. On the flip side, gut microbiota abnormalities in older adults are considered one risk factor for dementia.
References: Johns Hopkins Medicine, Enteric nervous system, PMC5808284, NPJ Science of Food, PMC7045475, Gut–brain axis and Parkinson's disease, Gut bacteria in toddlers

What's Living in Your Gut?
Think of your gut as a rich ecological forest, home to a massive population of microbes. How they're organized and balanced directly impacts your health.
The Numbers and Types of Gut Microbes
According to the U.S. National Institutes of Health Human Microbiome Project, a healthy adult gut contains:
- Hundreds to thousands of different bacterial species
- Tens of trillions of individual microbes
- A total weight of about 1-2 kg (similar to your brain's weight)
These microbes fall into three groups:
- Good bacteria (probiotics): Help with digestion, make vitamins, keep bad bacteria in check, and support your immune system
- Neutral bacteria (opportunistic): Usually harmless, but can turn problematic when your immunity drops or gut balance shifts
- Bad bacteria (pathogens): Cause trouble when they overpopulate
Here's the thing: balance matters. When good bacteria dominate, they keep bad bacteria suppressed—it's a healthy cycle. When balance tips the other way, health issues emerge.
Why Is Everyone's Gut Microbiota Unique?
Your gut microbiota is as unique as your fingerprint. Several factors shape its makeup:
| Factor | Can You Change It? | What It Means |
|---|---|---|
| Birth method | No | Babies born vaginally pick up their mother's microbiota through the birth canal, creating more diverse starting populations |
| Diet | Yes | Eating vegetables, fermented foods, and diverse diets nurtures good bacteria; high sugar and highly processed foods feed bad bacteria |
| Antibiotic use | Yes | Antibiotics wipe out both good and bad bacteria; use only when needed, and consider gut restoration afterward |
| Stress levels | Yes | Chronic stress changes your gut environment, affecting microbiota stability |
| Age | No | Microbiota diversity naturally drops with age, but lifestyle choices can slow this down |
(Swipe left/right to view full table on mobile)
The good news? Most of these factors are in your control. No matter your past, it's never too late to make changes.
What Is Gut Microbiota Imbalance?
"Microbiota imbalance" means your gut ecosystem is out of whack:
- Good bacteria decrease and diversity drops
- Bad bacteria or opportunistic bacteria increase
- Microbiota function gets disrupted
Five major culprits in modern life:
1. High-Sugar, High-Fat, Low-Fiber Diet
Refined sugars feed bad bacteria, letting them multiply quickly. Not enough fiber? Good bacteria starve.
2. Frequent or Inappropriate Antibiotic Use
Antibiotics kill bacteria without discrimination. One course can affect your gut for months or longer.
3. Chronic Long-Term Stress
Stress hormones mess with your gut environment, decreasing good bacteria while boosting bad ones. That's why you get diarrhea or constipation during exams or stressful work periods.
4. Sedentary Lifestyle or Lack of Exercise
Not moving enough reduces gut motility and microbiota diversity.
5. Environmental Toxins
Pesticide residues, food additives, and plasticizers all throw gut balance off.
Research shows indigenous people from remote tribes have more diverse gut microbiota than modern city dwellers. This "microbiota impoverishment" links to the rise of modern diseases like obesity, diabetes, and autoimmune conditions.
Key concept: Microbiota imbalance works like dominoes falling—it starts with gut inflammation, then progressively affects your immune, metabolic, and nervous systems. Restoring gut balance is key to preventing chronic diseases.
References: Human Microbiome Project, Cell 2016, PMC10699709, Science Alert, MDPI: life15121812, National Geographic
When Your Gut Is Out of Balance, Your Body Sends Warning Signs
Gut microbiota imbalance doesn't just mess with digestion—it affects systems throughout your body.
1. Immune System: Getting Sick More Often, More Allergies
Gut microbes play a key role in how your immune system matures and stays balanced. After birth, microbial colonization trains your immune system to tell friend from foe.
What happens when microbiota gets imbalanced:
- Chronic inflammation: Microbiota imbalance damages your gut barrier, letting toxins leak into your bloodstream and triggering body-wide inflammation
- Immune dysfunction: Can't fight off actual pathogens (hello, infections) while attacking your own cells (allergies, autoimmune conditions)
- Weakened defenses: Like a castle wall with holes—pathogens invade more easily
2. Mental and Emotional Health: Anxiety, Depression, and Poor Sleep
When microbiota gets imbalanced, neurotransmitter production gets disrupted. Naturally, your mood takes a hit.
What research shows:
- A significant number of IBS patients also face anxiety or depression
- People with depression show lower gut microbiota diversity; those with anxiety have fewer good bacteria and more inflammatory bacteria
- Animal studies: Mice without gut microbiota show anxious behavior; symptoms improve after probiotic supplementation
3. Weight and Metabolism: Higher Risk of Obesity and Type 2 Diabetes
Your gut microbiota affects how efficiently you metabolize food.
What science has found:
- Obese individuals have lower gut microbiota diversity, with some bacterial species better at "extracting" calories from food
- Type 2 diabetes patients have fewer good bacteria making short-chain fatty acids and lower microbiota diversity
Scientists ran "fecal transplant" experiments: transplanting gut microbiota from normal-weight people to obese individuals improved insulin sensitivity in the recipients. This shows that with identical diet and exercise, microbiota differences can affect metabolism and weight management.
4. Cardiovascular Health: The TMAO Risk
Eating too much red meat and egg yolks causes certain gut bacteria to metabolize them into "TMAO" (trimethylamine N-oxide).
Why TMAO is bad news:
- Promotes atherosclerosis and blood clot formation
- Considered a major risk factor for cardiovascular disease
- People with high TMAO levels face higher cardiovascular disease risk
Here's something interesting: vegetarians who occasionally eat red meat don't see TMAO spikes—because their microbiota composition differs. The key isn't just "what you eat" but also "how your gut microbiota metabolizes it."
5. Brain Health: Neurodegenerative Diseases
Links exist between your gut and neurodegenerative diseases.
Parkinson's disease patterns:
- Patients show about 77.6% reduction in "Prevotella" bacteria
- Constipation and other gut issues commonly show up early, potentially before motor symptoms
- Animal experiments: Transplanting Parkinson's patients' gut microbiota into mice causes motor impairments in the mice
- Research suggests gut bacteria imbalances might send harmful proteins to the brain via the vagus nerve
Alzheimer's disease:
Research found certain gut microbiota metabolites can cross the blood-brain barrier, worsening beta-amyloid protein buildup in the brain—one of Alzheimer's hallmarks.
6. Digestive System: IBS and GERD
Microbiota imbalance directly messes with gut function:
- Irritable Bowel Syndrome (IBS): Affects about 10% of people globally, with symptoms including abdominal pain, bloating, and alternating diarrhea or constipation
- Inflammatory Bowel Disease (IBD): Includes Crohn's disease and ulcerative colitis; studies show IBD patients have fewer good bacteria and more harmful bacteria
- Gastroesophageal reflux: Small intestinal bacterial overgrowth (SIBO) may be a contributing factor
- Colorectal cancer risk: Research links certain bacterial strains to colorectal cancer development
7. Skin Health: Acne and Eczema
The "gut-skin axis" exists—your gut microbiota status shows up on your skin.
What research shows:
- About 50% of skin disease patients also have gut symptoms
- Eczema, psoriasis, and acne patients often show reduced gut microbiota diversity
- Taking specific probiotics can improve acne symptoms
Imbalanced microbiota triggers body-wide inflammation. When gut permeability increases, toxins leak into your bloodstream, causing your skin (as a target organ) to show symptoms like itching and rashes.
Quick Summary
| System Affected | Common Symptoms/Conditions | Why It Happens |
|---|---|---|
| Immune | Frequent colds, allergies, autoimmune issues | Your gut contains tons of immune cells; imbalance weakens defenses |
| Mental | Anxiety, depression, insomnia | Gut-made neurotransmitters affect mood |
| Metabolic | Obesity, diabetes | Some bacterial populations extract more calories from food |
| Cardiovascular | Atherosclerosis, heart disease | Your gut produces harmful TMAO |
| Neurological | Parkinson's, dementia | Gut issues may show up before brain symptoms |
| Digestive | IBS, GERD | Microbiota imbalance directly affects digestion |
| Skin | Acne, eczema | Gut inflammation shows up on skin |
| Other | Recurrent vaginal yeast infections; Chronic bad breath | Microbiota dysregulation: Vaginal and gut yeast often grow together, starting in the gut (especially after multiple broad-spectrum antibiotic courses); Abnormal gut fermentation products get exhaled |
(Swipe left/right to view full table on mobile)
References: Hopkins Medicine:The Brain-Gut Connection, PMC11865252, PMC11953144, PMC10810176, PMC10699709, Science Direct: Gut microbiota & Heart, PMID: 23563705, PMID: 27776263, CancerBioMed: Tumorigenic bacteria in colorectal cancer, PMC8953587, PMC5418745, Cureus: The Impact of Probiotics on Acne Vulgaris
High-Risk Groups Checklist
| Situation | Risk Level | What to Do |
|---|---|---|
| Took antibiotics in the past 6 months | Very High | Take probiotics |
| Eat fast food/processed food 3+ times per week | High | Change diet habits |
| Eat less than 3 servings of fruits/vegetables daily | High | Up your fiber intake |
| Chronic diarrhea or constipation (>2-4 weeks) | High | Check gut function, see a doctor if needed |
| Frequent bloating, excessive gas, unusual odor | Moderate-High | Look at fermentation and microbiota status |
| High work or life stress | Moderate-High | Learn to relax, consider probiotics |
| Sleep less than 6 hours daily | Moderate | Make sleep a priority |
| Sit more than 8 hours daily | Moderate | Get more active |
| Long-term PPI (proton pump inhibitor) use | Moderate-High | Talk adjustments over with your doctor |
| Frequent colds, allergic reactions | Moderate-High | Support immunity through gut health |
| Age 50+ | Moderate | Boost microbiota diversity |
(Swipe left/right to view full table on mobile)
Important reminder: If gut symptoms stick around beyond 4 weeks, or if 3+ symptoms from different systems show up together, see a doctor.

Four Ways to Get Your Gut Back on Track
Restoring gut health is easier than you think. Plus, you can feel results pretty quickly.
Method 1: Adjust Your Diet—Feed the Right Bacteria, Build a Healthy Microbiome
| Goal | How to Do It | Good Choices | Tips & Tricks |
|---|---|---|---|
| Eat more: High fiber | Get enough fiber daily (aim for 25–35g per day) | Whole grains (oats, brown rice, quinoa), legumes (black beans, chickpeas), vegetables (broccoli, carrots, beets), fruits (berries, apples with skin, kiwi) | Make at least half your plate vegetables at each meal; swap white rice and white bread for whole grains; increase fiber gradually (to avoid bloating at first) |
| Eat more: Fermented foods (natural probiotics) | Add 1 type to your daily routine | Unsweetened yogurt, kefir, kimchi/sauerkraut, miso, natto, kombucha | Pick products "containing live cultures/unpasteurized"; skip high-sugar fermented drinks (sweet fermented drinks often disappoint) |
| Eat more: Prebiotics (feed good bacteria) | Use "specialized fiber for good bacteria" | Onions, garlic, leeks, asparagus, unripe bananas (yellow-green), oats | If you're prone to bloating at first: start small and spread throughout meals |
| Eat less: Refined sugar/high fructose | Cut back on sugary drinks, desserts, candy | — | Best to start with "beverages" (easiest to overconsume) |
| Eat less: Excessive red meat | Control red meat frequency and portion | Use fish, chicken, legumes as main protein | No more than 2–3 times per week; pairing with high-fiber diet matters more |
| Eat less: Artificial sweeteners (avoid disrupting microbiota) | Reduce dependence on aspartame, sucralose, etc. | — | Not "complete elimination," but use as a bridge and gradually cut sweetness |
| Eat less: Processed foods | Cut back on instant noodles, sausages, bacon, etc. | — | Focus on reducing "high-frequency processed items" rather than banning everything for better long-term success |
(Swipe left/right to view full table on mobile)
How to make it work: Use the "80/20 rule"—eat the right foods 80% of the time, enjoy treats 20% of the time. This approach sticks.
References: PMC9268622, Human Microbiome Project, PMC10699709, MDPI: life15121812, PMID: 23563705
Method 2: Improve Lifestyle Habits—Reduce Stress + Exercise + Sleep to Restore Microbiota Rhythm
Your lifestyle habits hit your gut microbiota more directly than you might think:
Stress Is Your Gut's Silent Enemy
Chronic stress links to microbiota changes and increased inflammation. Learn to relax so your gut can function normally.
Exercise Makes Your Microbiota Richer
Research shows athletes have more diverse gut microbiota than couch potatoes. Exercise doesn't just get your gut moving—it also produces lactic acid that changes gut pH to keep bad bacteria in check and lowers body-wide inflammation.
Sleep Affects Microbiota Rhythm
Your gut microbiota has its own circadian clock. Sleep loss or jet lag throws off the microbiota's day-night rhythm—studies show even short-term sleep restriction can change microbiota makeup and boost potentially harmful bacteria. Long-term sleep deprivation makes gut imbalance worse.
| Lifestyle Factor | What It Does | How to Do It |
|---|---|---|
| Reduce stress | Lower stress impact on gut motility, lining, and microbiota | Mindfulness meditation 10–20 min/day; deep breathing; regular outdoor time weekly |
| Regular exercise | Boost microbiota diversity, get things moving, cut inflammation | 150 minutes moderate intensity per week (can split into multiple 10–15 minute sessions, still works) |
| Avoid overdoing it | Prevent gut issues/intestinal wall damage from too much | Build up high-intensity exercise gradually; marathon/ultra-high intensity needs special attention to recovery and nutrition |
| Get enough sleep | Keep microbiota circadian rhythm, lower metabolic risk | 7–9 hours nightly; consistent sleep-wake times; sleep 3 hours after dinner; cut blue light before bed |
(Swipe left/right to view full table on mobile)
References: PMC11547208, PMC11260001, Frontiers in Neuroscience, PMC9896348, Science Direct: Gut microbial ecosystem & Exercise
Method 3: Use Medications Carefully—Protect Your Good Bacteria
Some common medications can harm gut bacteria. Use them carefully.
| Medication Type | What It Does | What to Do |
|---|---|---|
| Antibiotics | Mess up microbiota balance, effects last months or longer (broad-spectrum antibiotics seriously disrupt microbiota balance) | Common advice: use only when needed; finish the course; space probiotics several hours from antibiotics; keep taking probiotics for several weeks after stopping |
| PPI gastric medications | Reduced stomach acid lets bad bacteria into intestines more easily, increases SIBO risk | Go short-term over long-term; talk risks/alternatives over with your doctor if long-term use is needed |
| NSAIDs pain relievers (like ibuprofen) | May damage intestinal lining, increase permeability | Use lowest effective dose when needed; check gut risks if using long-term |
| Metformin | Changes microbiota (overall benefits beat drawbacks), may cause gut side effects | Follow doctor's orders; if diarrhea or other side effects are significant, discuss microbiota support with your doctor |
(Swipe left/right to view full table on mobile)
Bottom line: Talk to a doctor before taking medications; don't self-prescribe long-term. If long-term medication is needed, discuss whether to add probiotics.
References: PMC10699709, Cleveland Clinic
Method 4: Add Probiotics—"Seeds" to Speed Up Recovery
Key idea: The first three items (diet, lifestyle, medications) are your foundation. Probiotics are like adding quality seedlings to a well-kept garden—they help your ecosystem bounce back faster.
| Topic | What It Does | How to Do It |
|---|---|---|
| Where probiotics fit | Diet/lifestyle/medication are the foundation; probiotics are the "boost" | Get diet and daily habits to 60–80% compliance, then use probiotics to speed things up |
| When to add them | Five situations: 1. After antibiotic treatment 2. Gut discomfort lasting beyond 4 weeks 3. Recurrent colds, allergies 4. Chronic high stress, eating out a lot 5. Special groups (long-term medication users, elderly) | How to use them: - With antibiotics: take several hours apart - After stopping meds: keep taking for several weeks - Special groups: check with a pro first |
| How to pick products (5 points) | 1. Pick strains: Different strains do different things 2. Enough CFU count: CFU is "Colony Forming Units," shows live bacteria count; more isn't always better 3. Live bacteria protection tech: Probiotics are super sensitive to heat, moisture, and oxygen—need tech protection to stay alive 4. Paired with prebiotics: Probiotics + prebiotics called "Synbiotics" help probiotics survive and work better in your gut 5. Third-party testing |
①Products should list complete strain names (genus + species + strain code) with research backing ②Check "expiration guarantee count"; common ranges are billions to hundreds of billions, depends on strain and research (talk to your doctor) ③Key tech: Low-temp processing (avoids heat damage during making); Low water activity (puts bacteria in hibernation, extends life); Encapsulation/microencapsulation (protects bacteria through stomach acid); Sealed packaging (blocks light, oxygen, moisture) ④Common prebiotic ingredients: Inulin, fructooligosaccharides, galactooligosaccharides, resistant starch ⑤Third-party live bacteria count testing or stability reports |
| How long to use | Gut adjustment takes time; give it 3–6 months | Keep taking for 3–6 months + make diet/habit changes at the same time, then see if you notice a difference |
(Swipe left/right to view full table on mobile)
References: Cleveland Clinic, PMC12590280
Probiotics Can't Replace a Healthy Diet—They Boost Healthy Choices
Think about it this way:
- Bad diet + probiotics = Planting trees while cutting them down—limited results
- Healthy diet + probiotics = Rich soil plus quality seedlings—way better results
Best approach:
- First fix diet (vegetables, fermented foods)
- Improve lifestyle (stress, exercise, sleep)
- Add probiotics on this foundation
- Keep it up for 3-6 months to see results
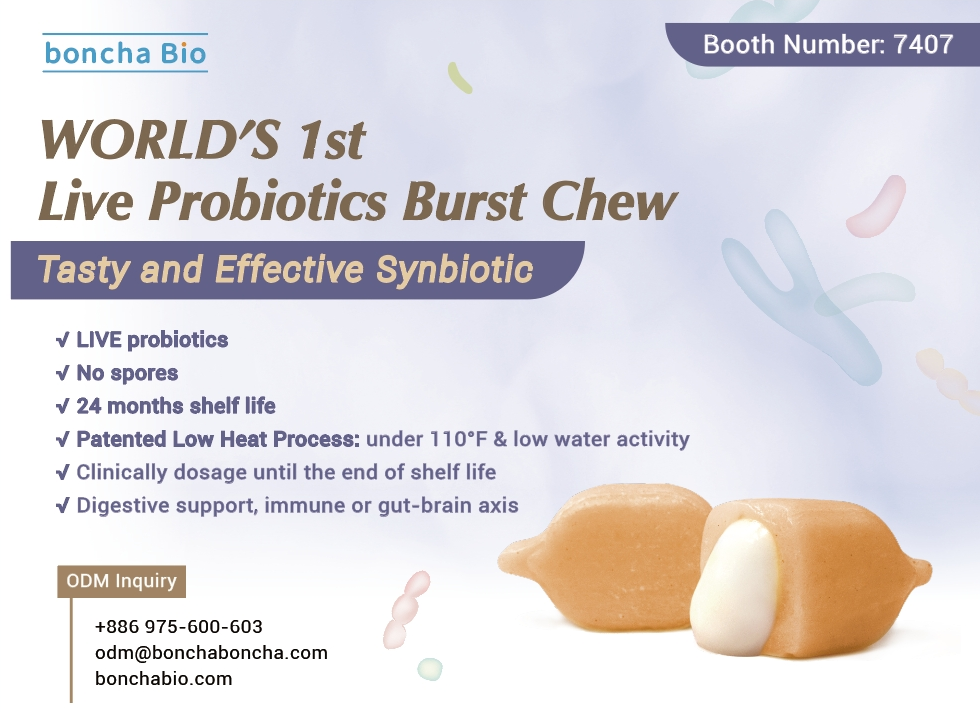
Boncha Bio—Making Sure Probiotics "Actually Reach Your Gut"
Boncha Bio's Solutions
Probiotic supplementation is just one piece of the gut health puzzle—diet, lifestyle, and stress management form the foundation. Probiotics are more like a boost that works better when the foundation is solid.
If you're going to supplement, every bacterium should "arrive alive in your gut" to deliver real benefits. We don't chase miracle products. Instead, we focus on solving the three core technical challenges in the probiotics industry.
Problem 1: Live Bacteria Die Off During Manufacturing and Storage
Common industry issues:
- Products labeled "10-30 billion CFU" may have less than half left by expiration
- Traditional processes using high heat and pressure kill live bacteria
- Bad storage (room temperature, humidity) speeds up death
Boncha's "Bacterial Hibernation" Tech: Giving Every Bacterium a Chance to "Arrive Alive in Your Gut"
- Low-temp, low-pressure processing: Controls manufacturing temperature to avoid heat damage
- Ultra-low water activity: Puts probiotics into hibernation, extending lifespan
Tech advantage: Keep bacteria alive first—only then can they work
Problem 2: Stomach Acid Creates a Harsh Environment for Live Bacteria
Common industry issues:
- Stomach acid pH of 1.5-3.5 is tough on most lactic acid bacteria
- Regular probiotics staying in the stomach see survival rates drop significantly in the acidic environment
- Powders and tablets get directly exposed to stomach acid without protection
Boncha's Solution | Chewable/Candy Capsule Dual Protection:
- Outer layer protective proprietary tech design boosts probiotic survival rates
- Inner filling encapsulation: Probiotics embedded in special matrix forming a protective barrier
- Smart release: Release in your gut's more neutral, friendly environment
Tech advantage: Not throwing bacteria into your stomach hoping for the best, but designing a safe route for probiotics to reach their destination.
Problem 3: Probiotics Reach Your Gut But "Have No Food"—Struggling to Colonize
Common industry issues:
- Most products only add bacteria while ignoring their "survival resources" in your gut
- Lack of prebiotics means even if live bacteria arrive, they struggle to reproduce stably
- Can't compete with existing microbiota, making long-term colonization tough
Boncha's ProbioBooster Prebiotic Formula:
- Adds prebiotics (inulin, fructooligosaccharides, etc.) to the formula
- Probiotics "bring their own food" to your gut with instant nutritional support
- Promotes growth of existing good bacteria for longer-lasting effects
Working together: Synbiotic concept—bacteria + nutrition together work better.
Boncha Bio, as a manufacturer specializing in innovative chewable/candy capsule supplement formats, provides full services from concept to market:
✓ Strain selection consulting: We recommend the best strain combinations based on target populations and goals
✓ Format tech support: Innovative formats like candy capsules/functional gummies ensuring live bacteria survival and great taste
✓ Formula optimization guidance: Complex formulas combining probiotics + prebiotics + other nutrients
✓ ODM/OEM manufacturing: GMP-certified facilities providing one-stop service from R&D, prototyping to mass production
If you're planning probiotic products or looking for an R&D and manufacturing partner who can integrate "strain strategy × format technology × formula integration," reach out to us.
Frequently Asked Questions
Q1. What is the gut-brain axis?
A: The gut-brain axis is a two-way communication system between your gut and brain through nerves, hormones, and immune signals affecting mood, sleep, and overall health, with 80% of signals flowing from gut to brain.
Q2. Why is your gut called the "second brain"?
A: Your gut contains hundreds of millions of nerve cells forming an independent nervous system and produces about 90% of your body's serotonin. When your gut isn't happy, your mood takes a hit.
Q3. What health problems can gut microbiota imbalance cause?
A: Microbiota imbalance affects seven major systems: weakened immunity, anxiety and depression, obesity and diabetes, cardiovascular disease, Parkinson's and dementia, IBS, and acne and eczema.
Q4. How can I tell if I'm in the high-risk group for gut health issues?
A: High-risk groups include: took antibiotics in past 6 months, eat fast food 3+ times weekly, under 3 fruit/vegetable servings daily, chronic digestive issues over 4 weeks, high stress with poor sleep, age 50+.
Q5. Where should I start to improve gut health?
A: Prioritize diet adjustments: 25-35g fiber daily (whole grains, vegetables, fruits), one fermented food (yogurt, kimchi), prebiotic foods (onions, garlic), and reduce refined sugar and processed foods.
Q6. What's the difference between probiotics and prebiotics?
A: Probiotics are live bacteria that add good bacteria to your gut; prebiotics are food for good bacteria. The best choice is "synbiotics"—combining both for better effects.
Q7. When do I need to take probiotics?
A: Five situations need supplementation: after antibiotics, gut discomfort over 4 weeks, recurrent colds or allergies, chronic high stress with frequent eating out, special groups like long-term medication users or elderly.
Q8. Why does stress cause gut problems?
A: Stress hormones decrease good bacteria by 25% and increase bad bacteria while reducing gut motility. Daily meditation 10-20 minutes, deep breathing, and weekly outdoor time help.
Q9. Can the gut microbiota recover from antibiotic damage?
A: Antibiotics severely disrupt microbiota with effects lasting months. Right approach: use only when needed, finish course, take probiotics 2-3 hours apart from antibiotics, continue 1-2 weeks after.
Q10. What makes Boncha Bio's probiotic technology special?
A: Boncha Bio solves three core challenges: bacterial hibernation tech ensures live bacteria count, chewable dual protection boosts survival rates, and ProbioBooster formula lets probiotics bring their own food for longer-lasting effects.
Extended Reading
Probiotic Series
- 《What Is Probiotic CFU? How to Choose the Right Probiotic for You?》
- 《Complete Guide to Probiotic Formats: Candy Formats for Better Taste and Absorption!》
- 《Candy Capsules vs. Functional Gummies: Differences and Selection Guide》
Related Health Topics
Article Classification
Recent Articles
- Bloated After Holiday Feasts? Your Guide to Beating Digestive Overload
- Is Your Gut Your Second Brain? How It Affects Your Whole Body
- Think Your Diet Is "Balanced"? 5 Nutrient Gaps 90% Miss and How a Multivitamin Can Help
- Brain Crashes Every Afternoon? You Might Be Dealing with Cognitive Fatigue
- 1 Billion People Affected by Vitamin D Deficiency (the “Sunshine Vitamin”)—Are You One of Them?


.jpg)